All in the Mind
No one expected the mice to simply drop dead.
But they did. Their sacrifice led to an encouraging new direction in Alzheimer’s research at the Emory laboratory of David Katz.
In another campus research project, Emory scientists led by Keqiang Ye 98PhD have identified a therapeutic compound that may arrest the progressive dementia associated with both Alzheimer’s disease and Parkinson’s disease.
While following different approaches, both projects are using basic science research to unpack the complex mechanisms underlying neurodegenerative disease and find ways to arrest it.
“The biggest risk factor for Alzheimer’s and other dementias is age, and we have an aging population,” observes Susan Peterson-Hazan, the Education Core coleader at the Alzheimer’s Disease Research Center (ADRC) and a licensed clinical social worker who coordinates Alzheimer’s family education programs offered by Emory.
The US Census Bureau reports that 49 million Americans are age sixty-five and over, a number projected to jump to 88.5 million by 2050. The number of Americans with Alzheimer’s, according to the Centers for Disease Control and Prevention (CDC), is expected to rise proportionately from 5.5 million in 2017 to nearly 14 million by 2050.
The impact of this massive public health dilemma will be felt in every corner of society and the economy, according to Peterson-Hazan, particularly in the health care industry, state and federal budgets, business, and in the financial well-being of family caregivers. Direct caregiving costs alone could reach $1.1 trillion annually by 2050, the CDC estimates.
Then there’s the emotional cost.
“It’s not unusual to see a family member drop off a loved one with Alzheimer’s at the emergency room, saying, ‘Doc, I can’t do it anymore. I know this isn’t the best thing, but there’s nothing else I can do,’ ” says Merrick “Rick” Lipman 95C 00M, an emergency room physician at the Veterans Administration (VA) Hospital in Decatur. “And it’s not just at the VA—this happens at community hospitals everywhere when family caregivers have reached their emotional and physical limit and don’t know what to do anymore.”
Says Peterson-Hazan, “If we can alter the course of the disease so it doesn’t progress, that would be an incredible gift to individuals, their families, and the community, and that’s of course the research goal.”
The gene lysine-specific demethylase 1 (LSD1) plays a critical role in the earliest stages of embryonic development by enabling undifferentiated cells, including stem cells, to turn into specific types of cells, such as neurons. It also serves an important regulatory function by ensuring that other genes that are supposed to be “off” remain so, thereby allowing embryos to develop correctly. Katz and his graduate students were studying the gene to learn more about how defects in the differentiation process may cause disease in the reproductive system.
In one early experiment, LSD1 was removed from a group of mice using genetic tools in combination with a “drug-inducible knockout system.” LSD1 was deleted from the intended target areas, but also from the mice brains.
The mice became cognitively impaired and paralyzed. Examination of their brains revealed changes in inflammation, cell metabolism, and cell communication consistent with Alzheimer’s disease and frontotemporal dementia (FTD), according to Katz.
At about the eight-week mark, all the mice died; it’s highly unusual for a gene-deletion procedure to result in death so quickly in adult mice.
Postmortem examination of the mice showed neurodegeneration and brain cell death in the hippocampus, the area of the brain associated with memory.
Perhaps even more remarkable, none of the mouse tissue samples contained the accumulation of sticky, toxic proteins—tau and beta-amyloid—generally considered to be the cause of dementia symptoms and cell death.
Following up with tissue samples from human Alzheimer’s and FTD patients, researchers found LSD1 embedded within the tangles of tau protein, but not in the nucleus where they belong, suggesting that cell death may not be caused exclusively by aggregates of tau and beta-amyloid after all, and instead are potentially related to LSD1 function.
“We stumbled onto something that nobody had considered,” says Katz. “We believe LSD1 could be either the major downstream component or maybe even the only downstream component for Alzheimer’s and FTD.”
The researchers hypothesized that neurons may require some kind of ongoing maintenance to remain viable and that this maintenance might be vulnerable to toxicity.
“Most people think that once a cell becomes a skin cell or a neuron or whatever, that’s it—you no longer need the DNA-packaging mechanisms that LSD1 provides for the initial cell differentiation,” Katz explains. “Our data suggests that cell type needs to be continually maintained—at least in the brain—and this function is carried out by LSD1.”
He likens the process to housekeeping.
“If you sweep the floor every day, you won’t get any dust buildup. But if you clean only once every few months, you’ll wind up with huge dust bunnies everywhere and your house will be a mess.”
Tau protein aggregates build up in the brain as part of the natural aging process. The trouble apparently begins when LSD1 is blocked from entering the nucleus and then lost through attenuation, which is why it was significant that LSD1 was found in the aggregates in the tissue samples of human Alzheimer’s patients.
Once stuck in the aggregate, “it can’t get to the genes where it’s supposed to be doing its housekeeping job,” Katz notes.
“We think downstream processes—immune responses, cell cycle, and all kinds of things that cells have to do—are affected in Alzheimer’s disease because LSD1 is affecting a lot of different neural pathways, specifically repressing genes in many of those pathways.”
The next phase of the research, Katz says, includes a series of experiments to identify a drug that will unstick LSD1 from the tau aggregates and force it back into neural nuclei, where it can perform its housekeeping function and prevent tau from killing neurons.
“LSD1 is a very interesting, completely novel target,” says Allan Levey, professor and chair of the Department of Neurology and director of the Emory ADRC. “There has been work over the past couple years suggesting that some other protein interactors with LSD1 in terms of regulating gene expression, particularly in development, may have an important role in Alzheimer’s disease. David’s work is the first to identify how important LSD1 is to that pathway and to neuron degeneration.”
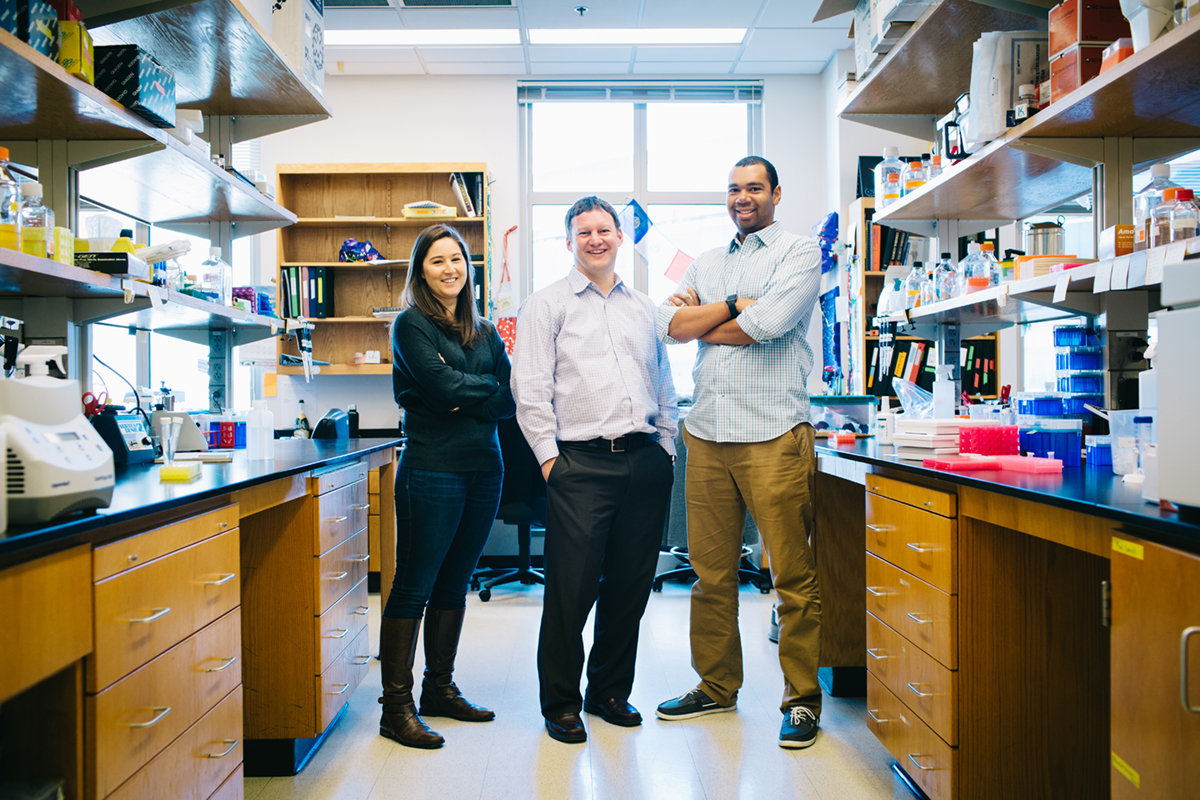
Brain Power: Neurologist David Katz (center) is doing groundbreaking research on Alzheimer's disease with doctoral students Amanda Engstrom (left) and Dexter Myrick.
Stephen Nowland
Pioneering university-level research relies in great measure on the initiative, insight, and hard work of graduate students.
At the Katz lab, “most of the actual day-to-day experiments have been done by graduate students under my direction,” says Katz.
In fact, the initial discovery that the loss of the protein LSD1 in the mouse brain causes neurodegeneration that looks similar to Alzheimer’s in humans was made by neuroscience doctoral student Dexter Myrick 10C 22PhD, who joined the Katz lab in 2010 as a technician and has continued working there as a grad student.
“It was originally a stem cell project that turned into a neuroscience project,” says Myrick. “I was working on a project investigating the loss of LSD1 in adult testis stem cells in the mouse. However, this mouse was lacking LSD1 in the rest of its body as well. We monitor all our mice regularly for general wellness, and during these routine checks I started making some peculiar observations. It wasn’t until the first mouse succumbed to what appeared to be a neurodegenerative disease that I really took notice. At this point, I began monitoring these mice very closely and examining their brain tissue postmortem. That is how we made the initial discovery that all these mice lacking LSD1 were undergoing progressive neurodegeneration.”
Myrick’s current role in the lab is to further investigate what LSD1 is doing mechanistically in neurons. Specifically, how LSD1 regulates transcription via histone methylation in hippocampus neurons.
“In our mice, we are directly manipulating LSD1 levels, but in human Alzheimer’s, we think the interaction between LSD1 and tau is significantly reducing the levels of LSD1 available to be used in the affected neurons.”
Soon after Myrick’s unexpected finding, Michael Christopher 16PhD joined the research effort in early April 2012 while a genetics and molecular biology doctoral candidate.
“I did experiments and drug delivery where we deleted LSD1 out of the mice,” Christopher says, “and then I would monitor the mice and help do all the experiments that described what happens to the mice when you get rid of LSD1. I also performed all of the staining of the human brain tissue samples we had.”
He and Myrick are co-first authors of the paper describing the research, “LSD1 Protects against Hippocampal and Cortical Neurodegeneration,” published in October 2017 in the journal Nature Communications.
After graduating, Christopher accepted a postdoc position at the University of California–Los Angeles, where he studies cellular function similar to LSD1, but in a different system not related to neurodegeneration.
Amanda Engstrom 22PhD, a biochemistry, cell, and developmental biology major whose background included cancer and diabetes research, was highly intrigued by the Katz lab project. So when Myrick and Christopher asked if she’d like to pick up on their work, she jumped at the opportunity—and became a convert
“I think it is super interesting,” says Engstrom. “I am also interested in pursuing a neuroscience postdoctoral fellowship, whereas I don’t think I would have considered that at all before.”
One of her projects in the Katz lab is investigating the specific interaction between tau and LSD1 that could lead to Alzheimer’s disease symptoms and neuronal cell death.
The shift in focus at Katz’s lab from stem cells to neurodegeneration required a tremendous amount of initiative on the part of his grad students, Katz says.
“Even the techniques they were doing were things that we had never done in our lab,” he continues, “so we all tried to learn as quickly as possible.”
With Myrick the only neuroscientist in the bunch, Christopher and Engstrom demonstrated praiseworthy willingness to venture outside the comfort of their respective fields. Both were allowed to take neurosciences classes even though they were not formally enrolled in the program, which reflected well on the neuroscience program, Katz points out.
The great thing about working in the Katz lab was that “we followed the science and didn’t put ourselves in any kind of box,” Myrick says. “That gives you a unique perspective.”
Engstrom agrees. “We’ve learned a lot more by not sticking with what we already knew and following the data to wherever it leads us.”
Alpha-synuclein is to Parkinson’s what tau and beta- amyloid are to Alzheimer’s—sticky, toxic proteins that accumulate in brain cells, fostering progressive dementia and other symptoms of their respective diseases, and eventually causing neuron death.
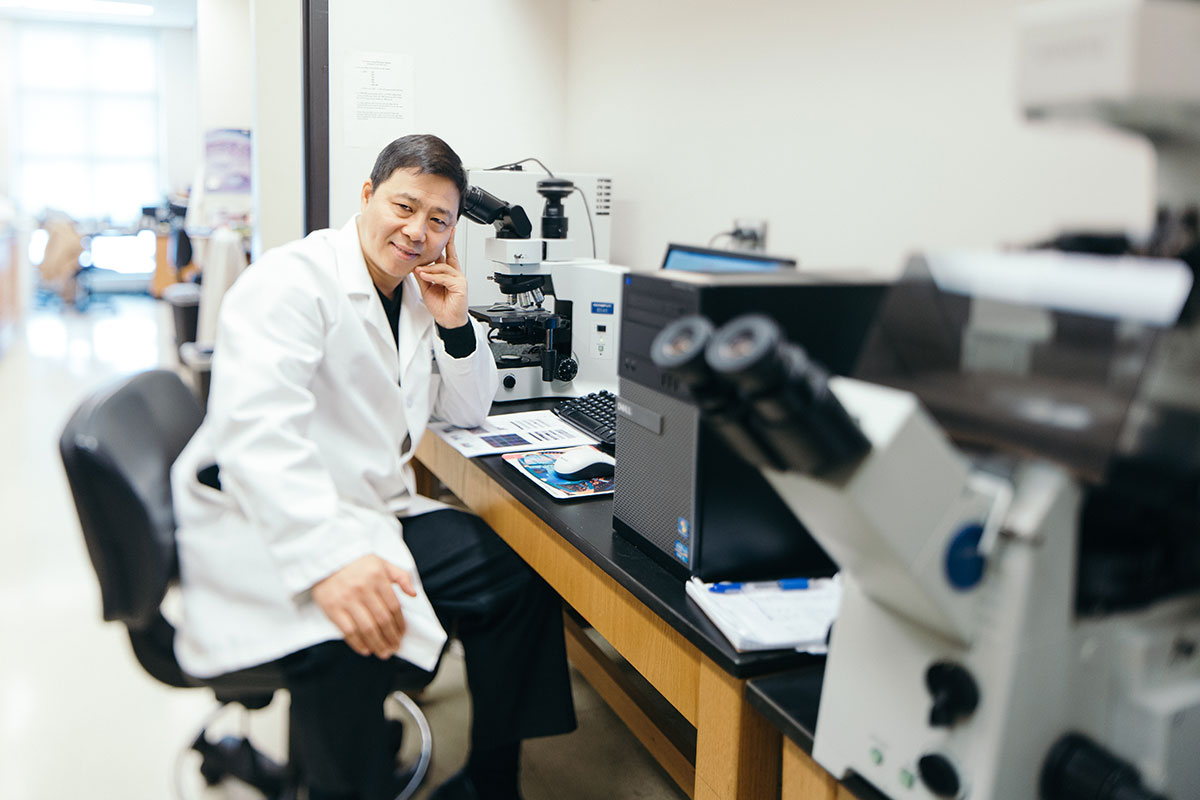
Brain Power: Emory researcher Keqiang Ye is working with the AEP enzyme to contribute to research for Alzheimer's.
Stephen Nowland
Keqiang Ye, a professor in the Department of Pathology and Laboratory Medicine, heads an Emory research team that discovered an enzyme that acts on these substances in ways that accelerate their spread and toxicity in the brain.
Finding drugs to inhibit this enzyme—asparagine endopeptidase (AEP), which normally digests unneeded molecules from cells—could lead to treatments that halt the neurodegeneration of Alzheimer’s, Parkinson’s, and other dementias, he says.
The research began eight years ago, when Zhixue Liu, Ye’s postdoc at the time, prepared an experiment to investigate DNase inhibitor apoptotic degradation and mistakenly used an acidic solution instead of a neutral solution.
The accident produced a key finding, that AEP was activated under acidic conditions, but not under conditions with a neutral pH.
Ye knew that AEP cuts tau into smaller pieces, more prone to clump together and more toxic. Further experimentation showed that AEP has a similar effect on the beta-amyloid present in Alzheimer’s. Ye reasoned that AEP might also cut the alpha-synuclein protein that affects the brain cells of Parkinson’s patients. He was right.
Brain tissue samples from Parkinson’s patients revealed the presence of alpha-synuclein fragments, but not in control samples. In addition, AEP was found throughout the neurons, though it is normally confined to a particular part of the cell.
Ye says the question then became: As the brain becomes more acidic with age, “will this enzyme be activated and play some role in neurodegeneration?”
His work with mouse models supports the hypothesis that AEP contributes to the progressive build-up of proteins characteristic of Alzheimer’s and Parkinson’s disease.
“If we block this enzyme with inhibitors, we may be able to slow down the pathology and rescue the cognitive functions associated with these diseases, and also reverse the motor dysfunction in Parkinson’s,” he elaborates.
This aspect of Ye’s research is detailed in the July 2017 online edition of Nature Structural and Molecular Biology.
“Dr. Ye is a prolific researcher who has embraced very big projects and has made a lot of progress across many fronts for Alzheimer’s and Parkinson’s disease,” ADRC’s Levey states. “He has been very successful developing therapeutic strategies based on his work.”
After screening about fifty-five thousand compounds, “We identified one brain-permeable compound that strongly inhibits the enzyme and prevents tau and alpha-synuclein cleavage in mouse models,” he says. “Now we are working on drug development and hope to initiate a clinical trial soon.”
Ye cautions against thinking of an AEP inhibitor as a possible cure-all. It’s not the only enzyme that cuts alpha-synuclein into small toxic pieces, and the full molecule can still aggregate and cause harm. Another unknown is whether an inhibited AEP would confer adverse effects on its waste-disposal function.
But given the urgency of finding effective treatments for Alzheimer’s and Parkinson’s, he believes the potential of this new approach is too exciting to not pursue.



